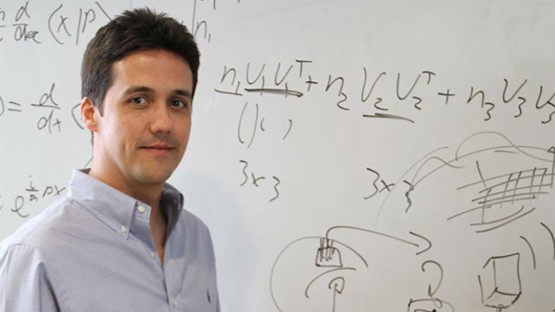
- He is a pioneer in the creation of brain-machine interfaces and a professor of electronic engineering and neuroscience at the prestigious University of California-Berkeley.
- «A person with a motor handicap will be able to move a robotic arm simply by thinking»
- Carmena will attend the Querer Foundation’s IV Neuroscientific and Educational Conference.
José Carmena is a Professor of Electronic Engineering Applied to Neuroscience at the renowned University of California-Berkeley, where he has been a professor and researcher for nearly two decades. Carmena is also a pioneer in the creation of brain-machine interfaces, which allow direct contact between the brain and an external device, such as a robotic arm or a prosthesis, in order to restore motor function in persons with disabilities.
In 2017, he founded the biotechnology firm iota Biosciences with the goal of turning research into a product that has a tangible impact on society. Similarly, he is a member of the team that will advise on the establishment of the National Neurotechnology Center ‘Spain Neurotech,’ which intends to become a world reference for the use of artificial intelligence to neurotechnology.
Carmena will travel from California to Madrid this month to participate in the IV Neuroscientific and Educational Conference organized by the Fundación Querer, where he will share his extensive knowledge about brain-machine interfaces and their applications in motor system diseases. He will be awarded the ‘Hero International Award’ for his prestigious international career in the change of Electronic Engineering and Neuroscience.
Question: Congratulations on your award. What does receiving the Fundación Querer’s ‘International Hero Award’ mean to you?
Answer: It is a tremendous honor, and it was completely unexpected. I’m looking forward to the conference because I know other speakers and it’s always nice to meet colleagues and people you appreciate. And most importantly, because I find the Fundación Querer’s mission and vision to be extremely interesting.
Q: In your lecture, you will discuss brain-machine interfaces and their applications in motor system illnesses, a specialty of yours. Why did you decide to commit yourself to research in this field?
A: Because it met my two primary motivations. On the one hand, there is the vocational one, which stems from having a family of doctors, of doing something clinically applicable for individuals with disabilities. That is, putting technology to good use for society. The other, strictly scientific, is my interest in learning how the brain works. In this situation, brain-machine interface technology is being used as an experimental paradigm.
«The brain-machine interface has the potential to improve the quality of life of many patients suffering from motor, sensory, and cognitive diseases.»
Q: For those who are unfamiliar with the subject. What is the functioning of a brain-machine interface?
A: First, there is a technology implanted (invasive) or not implanted (non-invasive) in the brain that records neuronal activity. The non-invasive method uses electroencephalogram (EEG) technology and electrodes implanted on the scalp, whereas the invasive method involves creating a craniotomy of the skull and inserting electrodes into the cerebral cortex. Of course, this does not cause pain in the brain.
The neuron inputs are then translated into motor signals by a mathematical algorithm, which controls a robot to complete a certain task. For example, imagine operating a robotic arm with your mind to grab for a glass of water. The concept is that a patient who is unable to move his arm but has a functioning brain can learn to operate a robotic arm simply by thinking about how he wants to do it.
Q: This procedure requires extensive training…
A: Yes, there is a critical component called feedback. The visual option is the most direct and straightforward in this scenario. The patient observes how effectively or poorly he does the task. By seeing the error that the brain makes, it can use it to repair that error and do it better the following time. The patient’s condition appears to be improving over time. This allows us to investigate neural plasticity and how the patient improves his or her control of the robotic arm. He will eventually learn and become an expert at controlling it.
Q: A brain-machine interface is a device that allows the brain to ‘control’ a robot while simultaneously allowing it to ‘sense’ the machine?
A: Yes, including tactile sense to increase control is a step forward. That is, in addition to being able to move that robotic arm, having that artificial body more integrated allows you to feel what the robotic hand grasps and so make a more exact grip. As an example, if I am going to shake someone’s hand, it is crucial for them to be able to experience the tactile sensations so that they do not squeeze too tight. It is critical to do both decoding and encoding of those artificial touch sensations back to the brain.
Q: Can you use the brain-machine interface to control devices other than robotic arms and legs?
A: Another common task is manipulating a cursor by staring at a computer screen and performing actions such as writing or drawing with that cursor. That is something you can do with mind. This has been demonstrated in several investigations, both in monkeys and in human patients.
“You could talk to Siri literally with your thought, without having to speak and much faster”
Q: What categories of people with disabilities might benefit from this technology, and how?
A: It has the potential to improve the quality of life for many persons with motor handicaps. It also helps with sensory and cognitive disorders in addition to motor problems. Even in speech. The most recent advancement, which was made a few months ago, is to use this technology with the motor activity of desiring to talk when the person is unable to do it. With merely thought and a lot of artificial intelligence, the muscle signals of what the patient wishes to communicate can be very faithfully interpreted. That is, you could literally converse to Siri with your thoughts, rather than speaking, and far faster. There are currently firms working on non-invasive techniques for this, not just for those with disabilities. On the other hand, there are companies dedicated to exploiting brain-machine interfaces in implants as memory prosthesis for persons who, for example, have memory impairments as a result of a stroke.
Q: What applications might it have for those who are not disabled?
A: It can improve specific functions in addition to repairing sensory, motor, or cognitive disorders. Nowadays, for example, there are prosthesis for persons who have had their legs amputated that allow them to compete with normal athletes since they can reach astonishing speeds and are more strong than real legs. Also, although I don’t see a use for it right now, having a visual prosthesis that stimulates your visual cortex so that you may train your brain to detect the infrared spectrum would be useful. For example, in terms of memory, being able to store many more things in the brain than we can. These final two are still science fiction, although neurotechnology is heading in that direction.
Q: What are the most difficult challenges that researchers encounter in developing and applying this form of brain-machine interface?
A: A critical issue that is currently being debated is the ethics of neurotechnologies, commonly referred to as “neuroethics.” The ethical issues, for example, for those without disabilities to use technologies due to the consequence of inequality that it can cause in society by dividing people into two classes, those who are augmented and those who are not. Then there could be data protection issues for those with disabilities. If the advancement of artificial intelligence is already a problem due to its power, when combined with neural implants in the brain, everything is compounded.
Q: In 2017, you created the biotechnology startup iota Biosciences. What kinds of devices do they create?
A: We are concentrating on neurotechnology, which consists of sensors or stimulators for the brain or any other portion of the body. Sensors to monitor oxygen in the blood, temperature, pH, blood pressure, or any parameter in an organ, for example, or to activate electrical activity in a nerve in the body. It is the field of bioelectric medicine, which is broader than only the brain-machine interface for robot motor control. We’re talking about linking all of the information highways that run through your body, from the brain to your extremities, all the way through your nervous system to an organ.
Q: All of this technology, particularly brain-machine interfaces, is expensive. How are you ensuring that it is accessible to all?
A: For the time being, this technology is largely used in clinical settings, where health insurance is expected to cover it, similar to when you have a liver transplant or an electrical stimulation implant for Parkinson’s. They are extremely expensive items that Social Security or the insurance that each individual has is intended to cover, or at least partially cover. In principle, that is the finance approach. And now, if it is about increasing capacity, there will be those that are more expensive and that insurance will not cover because it is merely a “whim,” but that is an ethical dilemma that must be seen and handled because it exists.